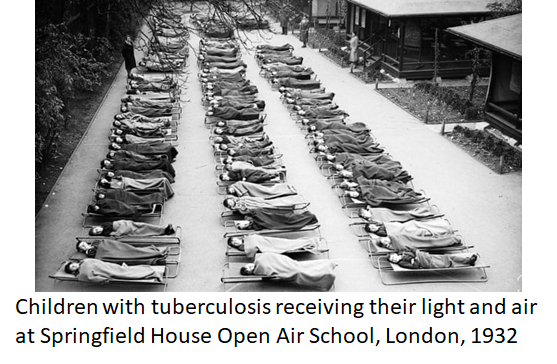
Modernist architecture in the early 20th century adopted the Licht und Luft principle, maximising light and ventilation to combat tuberculosis. Amid another airborne...
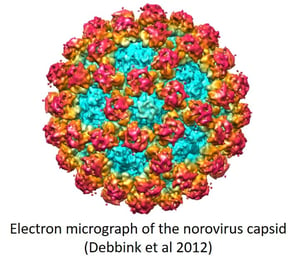
The winter vomiting bug is caused by the norovirus which spreads rapidly through aerosols and surfaces, survives for days or weeks between human hosts and is resistant to ammonia and alcohol-based cleaning products. We suggest that ultraviolet could be used to control its spread, especially public toilets and restaurants.
This article is part of a series on viruses in the built environment, which is a companion to the article on the suite of applications that Atamate is developing to mitigate their effects.
Viruses indoors 1: the urban incubator
Viruses indoors 2: Licht und Luft
Viruses indoors 3: Introducing the common cold
Viruses indoors 4: the flu season
 So far, this series has concentrated on how our built environment has proved to be too friendly to respiratory viruses like those that cause COVID-19 and the common cold and what we can do about it. Here we're going to talk about how the same set of issues apply to norovirus, often called the winter vomiting bug.
So far, this series has concentrated on how our built environment has proved to be too friendly to respiratory viruses like those that cause COVID-19 and the common cold and what we can do about it. Here we're going to talk about how the same set of issues apply to norovirus, often called the winter vomiting bug.
In the mid-1990s, some very brave scientists from the Food Standards Agency were immersed in the smelly stuff. They wanted to know what viruses and bacteria caused what they called 'intestinal infectious disease' but others might call gastroenteritis, food poisoning, gippy tummy or simply the shits. The latter term gives a clue to their approach: they collected stool samples from thousands of people suffering from the much-euphemised condition and used various approaches to see what nasties were hiding in them. It can't have been a pleasant task so we can only imagine their disappointment when they couldn't find any particular reason for nearly half their cases [PDF].
Scientists are notorious for preferring to leave freezers packed full of unappetising samples than to throw anything away and there's a good reason for that. The techniques for identifying microbes improved over the following decade and allowed a different group of scientists to return to the mystery samples with their shiny new tools.
What they found came as a surprise. Most of the mystery cases had been caused by a single virus, which made it responsible for a third of all cases of gastroenteritis. That made it the most important single cause of all gastroenteritis.
That virus was the norovirus.
 We now know the norovirus as the winter vomiting bug because it turned out to be at its most common in the winter. If we find ourselves unwilling to stray too far from the nearest toilet in the winter, there's a good chance that it's norovirus.
We now know the norovirus as the winter vomiting bug because it turned out to be at its most common in the winter. If we find ourselves unwilling to stray too far from the nearest toilet in the winter, there's a good chance that it's norovirus.
Once public health scientists knew to look for norovirus, they found it all over the place. Clarence Tam, then at the London School of Hygiene and Tropical Medicine, led a study to estimate the impact of norovirus in the UK over one year from 2008-2009. He found that norovirus infections sent around 130,000 people to their GPs and nearly 30,000 to accident and emergency, from which he extrapolated that around three million people were ill with norovirus even if the majority didn't see a doctor about it.
He estimated the cost to the NHS to be £11.9-17.7 million (£16.1-23.9 million inflation adjusted to 2019) but because most people might take a few days off work to recover or to care for a vomiting child, the total cost to the people who had been infected was much higher at £69 million (£93 million inflation adjusted to 2019). That makes for a total cost to the economy in the ballpark of £85 million which, for context, is around twice Vodafone UK's 2019 revenue [PDF] and twice the amount of public money spent on London's Garden Bridge project before it was terminated.
The effect of norovirus is eyewatering in more ways than one.
Once the importance of norovirus to both the stomach and the wallet was appreciated, a lot more research was focused on learning more about it and that research uncovered two key facts about it: it's very good at infecting people and it's very resilient when it’s between them.
The norovirus has a number of ways of spreading. It may be spread through the water supply and like most water-born viruses, it takes very few virus particles to establish an infection. Modern sanitation systems have largely closed the door on transmission through the water but as with respiratory viruses, modern living has helped it along in other, frankly revolting, ways.
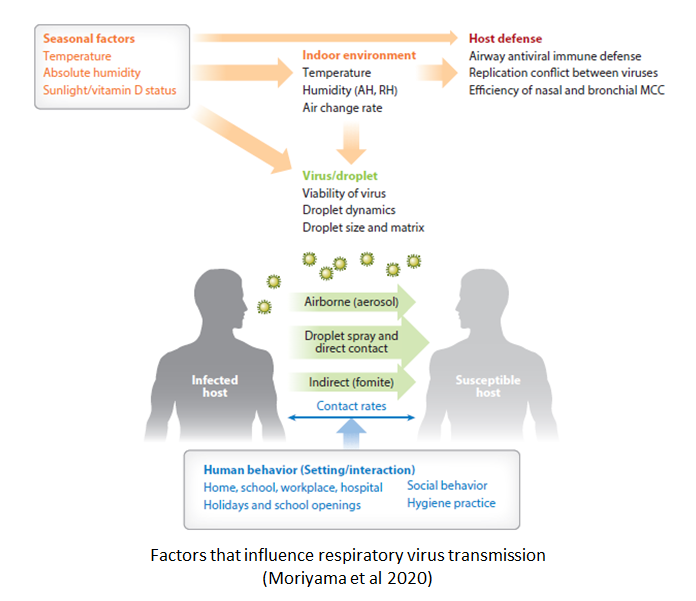
 One of those ways is by floating through the air in the form of an aerosol. When someone with winter vomiting bug vomits, they spew out fine droplets containing the virus that can stay suspended in the air for hours. If that's not nauseating enough, there is also a strong probability that it is spread through toilet plumes, which are the fine droplets that we launch into the air when we flush a toilet without closing the lid.
One of those ways is by floating through the air in the form of an aerosol. When someone with winter vomiting bug vomits, they spew out fine droplets containing the virus that can stay suspended in the air for hours. If that's not nauseating enough, there is also a strong probability that it is spread through toilet plumes, which are the fine droplets that we launch into the air when we flush a toilet without closing the lid.
Whichever end of the digestive system it originates from, norovirus carried by aerosols can be suspended in the air and can travel a long way. Anyone who inhales it will be infected but it will probably end up settling on a surface somewhere.
If that surface happens to be the surface of someone's meal, whoever eats it may be in for a nasty surprise a few hours later. If it's a surface used for food preparation, the virus easily transfers to any food placed on that surface. What makes it a particularly tricky customer is that the norovirus can survive for a long time in between hosts. While the COVID-19 virus doesn't last more than three days on a surface, noroviruses may last up to a month.
Once someone is infected, it may take a a few hours or a couple of days before the stomach cramps start. That's often as bad as it gets but it can progress to vomiting or diarrhoea. It usually clears up after two or three days although it can last for up to a week, especially in children.
Unpleasant and painful as it is, a saving grace of norovirus is that even the most severe cases do usually resolve. There's no treatment for the virus itself but if someone has a particularly severe case, a hospital can make sure that they stay hydrated and keep any other conditions under control until their own immune system gets rid of the virus. For people without that sort of hospital treatment available, the outlook can be less optimistic. Norovirus kills over 200,000 people every year, mostly children in low-income countries.
As with the respiratory virus infections, the immune system retains a memory of the virus and stops it infecting again. Different respiratory viruses have various tricks to get around our immune memory; for instance the coronaviruses stop the memory forming properly so they can infect again after a few years while the influenza viruses keep mutating so that after a few years, they're effectively a different virus to the one they left a memory of.
 Unfortunately, norovirus is adept at both of those tricks. Not only does it avoid leaving long-lasting immune memory but it mutates at a rate that leaves the immune memory effectively irrelevant. There are multiple strains of norovirus circulating at any given time and while a new 'pandemic' influenza that is completely different to anything we're immune to emerges every few decades, a new pandemic norovirus emerges every 2-4 years.
Unfortunately, norovirus is adept at both of those tricks. Not only does it avoid leaving long-lasting immune memory but it mutates at a rate that leaves the immune memory effectively irrelevant. There are multiple strains of norovirus circulating at any given time and while a new 'pandemic' influenza that is completely different to anything we're immune to emerges every few decades, a new pandemic norovirus emerges every 2-4 years.
Given how fast and how far it can spread, a norovirus can tear through a hospital or care home full of highly vulnerable people in a matter of days. It is also a major concern wherever there's food involved. One customer in a restaurant can fill in with aerosolised norovirus, with or without the aid of the toilet, that everyone else will blame on the restaurant's poor hygiene.
Norovirus's rapid mutation makes it very unlikely that there will be a vaccine in the foreseeable future so it needs to be done the old fashioned way: elbow grease and cleaning fluids. Even here, it manages to be frustrating in several ways.
The usual approach to testing a cleaning product against a virus is to inoculate a test surface with the virus in question, clean the surface with the test product and then try to culture virus from that  surface. If you can culture virus from an uncleaned surface but not a cleaned one, the cleaning product has killed the virus.
surface. If you can culture virus from an uncleaned surface but not a cleaned one, the cleaning product has killed the virus.
Testing cleaning products against norovirus has proved difficult because it was only in the last few years that the research group of Mary Estes at Baylor College of Medicine developed a way to culture norovirus. Their achievement is a major breakthrough in norovirus research that will be very significant going forward but for now, most of the research we have to draw on was done before Estes's team had developed their technique. Earlier research used the fact that it was possible to culture closely related members of the calicivirus family. There are viruses that infect cats and mice that have essentially the same structure as norovirus, meaning they would have the same vulnerability to difficult chemicals, and which could be cultures in the laboratory.
It turns out that caliciviruses are far more resilient to common cleaning products than most other virus families. Chlorine-based bleach is effective at clearing surfaces but ammonia and detergent-based cleaners were far less so. Even when chlorine was used, it wasn't enough to simply spray down a surface. It needed to be thoroughly wiped clean which suggests that it takes direct contact with at least 200ppm chlorine to be sure of killing a virus.
That finding also has relevance to the problem of toilet plumes: putting a bleach block in the tank may not give a high enough concentration to sterilise the water.
When it came to washing hands, the best option was thorough washing with soap and water.

Alcohol-based hand sanitisers were only effective at concentrations higher than the 60% of the typical over-the-counter products.
For as long as there's a danger of norovirus-laden aerosols drifting in, the only w
ay to keep a surface clean is to keep wiping it down with bleach but even that won't protect against the aerosols themselves.
Caliciviruses may be tough nuts for chemicals to crack but they do have a key weakness: they're very vulnerable to ultraviolet light. We design our indoor spaces to exclude ultraviolet which removes one of the few effective barriers to its spread but as we've said elsewhere, it's possible to use ultraviolet light in the indoor environment in ways that expose viruses but not humans.
Ultraviolet is already used in food preparation. Food is passed under pulsed xenon lamps that emit light across the spectrum from ultraviolet to infra-red, although it's only the ultraviolet wavelength that affects the viruses.
Atamate is currently developing an occupancy controlled ultraviolet disinfection system that can be fitted to a room and switches on whenever the room is empty, disinfecting any aerosols in the room and on surfaces. In certain circumstances, that could be combined with the established approach of upper-room ultraviolet, in which an ultraviolet lamp is set above head height and baffles protect people from being exposed to it.
To see how ultraviolet might be deployed against norovirus, let's consider something that we'd probably rather not contemplate more than absolutely necessary: the gents' toilets next to the food hall of a large shopping centre.
Whenever a toilets is flushed, it sends a plume of aerosols directed upward by the shape of the bowl and the walls of the cubicle and then it spreads through the whole of the room and out toward the food hall. If upper-room ultraviolet was fitted above the cubicles, that plume would be carrying norovirus or anything else unwholesome straight into a killing zone where most of it would be inactivated before it got anywhere near anyone else.
Some of the plume would stay below the killing zone, sipping out through the cubicle door to settle

on door handles or near the sinks where it might be touched or worse, sneak out into the food hall. However, a feature of public toilets is that occupancy is intermittent. Quite often, there's no one in there which is when occupancy control could flood the entire room with ultraviolet, disinfecting doorhandles and sinks before anyone can pick up any norovirus settled there and also inactivating any of it floating around as aerosols before it can find its way into the food hall.
If someone were to come into the gents' while disinfection was in progress, the occupancy control would switch it off so he would not be exposed. The whole system would effectively operate itself, keeping customers and cleaners alike safe from norovirus even if none of them notice it operating.
The food hall toilet is only one possible application of such a system and, as we've discussed, ultraviolet is equally effective against the respiratory viruses that cause COVID-19 and the common cold. We don't expect to be able to eradicate the norovirus any time soon but we do expect that using ultraviolet light can save us from a few bouts of winter vomiting.
If you’d like to know more about how Atamate Building Intelligence can support the wellbeing of the people who live and work in the urban environment, ask us on the form and we'll be happy to discuss it.
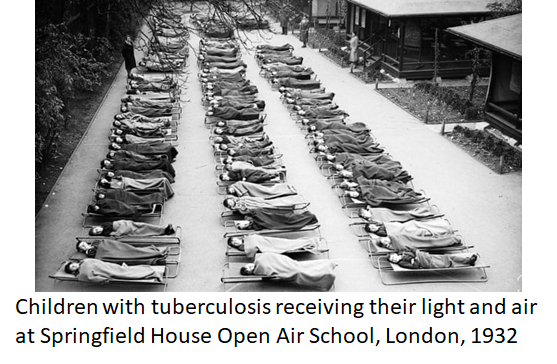
Modernist architecture in the early 20th century adopted the Licht und Luft principle, maximising light and ventilation to combat tuberculosis. Amid another airborne...
The modern urban environment is ideal for the transmission of respiratory viruses, which is why the common cold spreads so fast. COVID-19 spreads using the same...